Psychedelic Therapy for Veterans: A Healing Path Forward
The military transition is often described as a journey—but for many veterans, it feels more like being thrown into a storm without a compass. Loss of identity, trauma from service, and a lack of effective support systems can lead to isolation, depression, and even suicidal ideation. While traditional treatment options like antidepressants and talk therapy help some, many veterans find these methods insufficient. That’s why psychedelic therapy for veterans is gaining national attention as an innovative, science-backed solution.
In a powerful episode of VET S.O.S. "The Scoop," host Kings interviews Matt Zemon, a thought leader in the psychedelic space, about how alternative therapies are changing lives and bringing real hope to veterans who have run out of options.
The Journey Begins with Awareness
Matt Zemon is the bestselling author of The Veterans Guide to Psychedelics and a respected voice in the fields of neuroscience and mental health. His TED Talk, Psychedelics Are Catalysts, Not Cures, has reached over a million viewers, and his work sits at the intersection of science and spirituality.
Matt didn’t start out advocating for psychedelics. His own transformative experiences led him to pursue a master’s degree in psychology and neuroscience, and his path has since focused on how these powerful substances can be used ethically and safely—especially to address veteran trauma.
According to Matt, “Veterans are not broken. They just need more tools. Psychedelic therapy for veterans isn't about escaping reality—it's about confronting it in a way that leads to lasting healing.”
Why Psychedelic Therapy for Veterans Matters
Military service often comes with intense experiences—combat trauma, traumatic brain injuries, and loss of comrades—that leave deep psychological scars. Veterans may find themselves in a cycle of guilt, shame, and emotional shutdown. And for many, standard treatments just don’t go far enough.
This is where psychedelic therapy for veterans plays a critical role. Substances like ketamine, psilocybin, MDMA, and ayahuasca have shown promise in treating PTSD, depression, and anxiety—especially when paired with professional preparation and post-treatment integration.
Matt emphasizes that these aren’t "party drugs." Used in the right settings, they can break mental health cycles that trap veterans in emotional pain. “Psychedelics help us get underneath the symptoms and actually process trauma,” he explains. “We’re not numbing it anymore—we’re facing it.”
Stories of Transformation
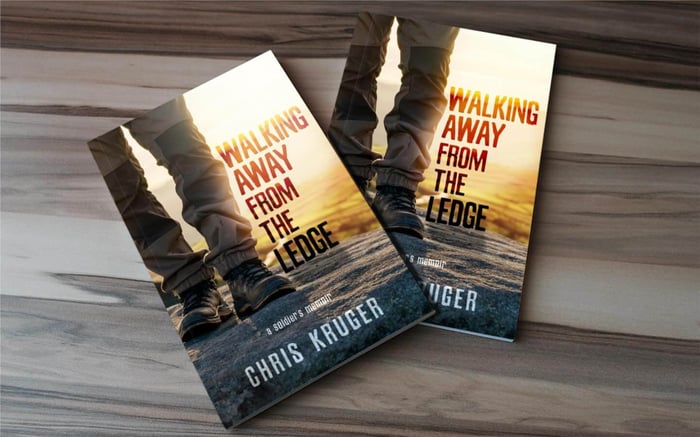
Host Kings shares his personal battle with post-service mental health, including severe weight gain and isolation after retiring from the military. At one point, he weighed over 400 pounds and couldn’t find motivation to move forward. Nothing seemed to work—until he read Matt’s book and saw himself reflected in its stories.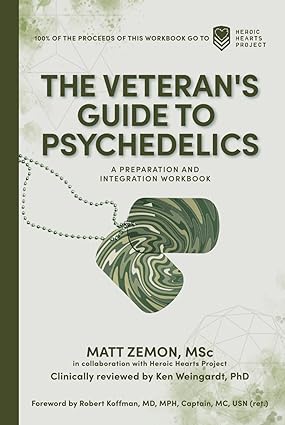
“The book helped me realize I wasn’t alone,” Kings says. “It felt like Matt was speaking directly to my experience. I needed something different—something deeper. Psychedelic therapy gave me hope I didn’t know I needed.”
Stories like this are becoming more common as veterans look beyond traditional VA resources and explore psychedelic options with the support of organizations like Heroic Hearts Project and The Mission Within, which offer scholarship-funded retreats.
Preparation Is Key
According to Matt, psychedelic therapy for veterans isn’t about taking a pill and hoping for the best. It requires intention, education, and mental and spiritual readiness.
“You’ve trained your whole career to prepare,” he says. “This is no different. You need to ask: Why now? What do I want to gain? What support will I need during and after?”
His book includes tools like a Life Satisfaction Tracker, gratitude journaling prompts, and comparison guides between substances like ketamine and MDMA. It walks veterans through the process of choosing the right environment—be it clinical, ceremonial, or spiritual—and ensuring they’re supported throughout.
Dispelling the Stigma
One of the major obstacles to adoption of psychedelic therapy is the lingering stigma from decades of drug prohibition and media fearmongering. Many veterans associate psychedelics with addiction or brain damage. But current research proves otherwise.
“When used intentionally, these medicines are non-addictive and non-toxic,” Matt explains. “The real risk is letting outdated fears stop people from healing.”
In fact, studies have shown that MDMA-assisted therapy, for example, can dramatically reduce symptoms of PTSD in veterans. And psilocybin has been linked to lasting improvements in mood, purpose, and resilience.
Matt’s mission is to demystify psychedelic therapy and show how it can be integrated into a comprehensive wellness plan for veterans.
Cultural and Ancestral Roots
Interestingly, Matt also points out that psychedelic therapy for veterans is not a new concept—it’s a return to ancestral healing. From Native American peyote ceremonies to African and Caribbean plant traditions, cultures around the world have used psychedelics for centuries to treat the soul.
Kings, whose family is from Belize and the West Indies, connects with this message deeply. “Growing up, we always had natural remedies for everything,” he says. “This isn’t a trend—it’s a return to something our ancestors knew.”
By reclaiming these practices in a modern, informed way, veterans can find healing that resonates not just scientifically, but spiritually.
Integration: Where the Real Work Happens
Psychedelic therapy doesn’t end with the session—it begins there. Integration is the most crucial phase, where the lessons learned during the experience are unpacked, digested, and implemented into daily life.
“Integration is about surrounding yourself with the right people,” Matt says. “Friends, coaches, therapists—people who can remind you of your worth when you forget.”
The post-psychedelic window of neuroplasticity—lasting roughly four weeks—is a golden opportunity for positive behavioral change. During this time, journaling, physical exercise, community involvement, and creative play (like coloring) can help veterans build new, healthier thought patterns.
Where Veterans Can Start
For those ready to explore psychedelic therapy for veterans, there are several accessible pathways:
Ketamine Clinics – Available legally in all 50 states.
Clinical Trials – Offered through universities and research hospitals.
Ceremonial Retreats – In countries like Peru, Mexico, and now Oregon.
Faith-Based Experiences – Legal under religious freedom protections in the U.S.
Organizations like Heroic Hearts Project offer fully-funded psychedelic retreats to veterans in need. “If you can’t pay, they’ve got you,” Matt says. “And if you can, you’re invited to pay it forward.”
A New Chapter in Veteran Healing
At the end of the day, psychedelic therapy for veterans is not a magic bullet—but it is a powerful tool. It’s a chance to break old patterns, face deep-seated trauma, and emerge with clarity, self-compassion, and direction.
As Kings says in the episode, “I tell myself every morning, ‘Make your dash count.’ I’ve been through the darkness—but now I’m choosing to lead others out.”
For veterans looking for a new beginning, psychedelic therapy may be the path they’ve been waiting for.
Resources Mentioned:
📖 The Veterans Guide to Psychedelics – Available on Amazon
🌐 Learn more: www.mattzemon.com
🧠 Scholarships for retreats: www.heroicheartsproject.org
🎤 TEDx Talk: Psychedelics Are Catalysts, Not Cures